The Headache & Migraine Policy Forum and Alliance for Headache Disorders Advocacy hosted “Women’s Headache Health Through Life Stages,” a discussion on how federal policy can support optimal migraine management in all life stages.
Migraine patient and advocate Justina Martin talks about her success with patient access.
Migraine and headache disorders disproportionately affect women during their childbearing and working years. But women may experience migraine disease throughout their lives.
What happens when migraine patients can’t access the medication they’re prescribed? Many must resort to hospital emergency departments for acute care during attacks, data show. In fact, migraine patients are the fourth highest users of the emergency department.
Migraine care is constantly evolving.
Advocates can use the resources in this toolkit to raise awareness and work together toward improving access to preventive treatments.
Migraine and headache advocates are a powerful force for change. In response to onerous step therapy requirements, The Headache & Migraine Policy Forum joined with partners and coalition members to improve access to CGRP inhibitors. Direct advocacy succeeded in reducing barriers in two states.
Medicare beneficiaries may soon be able to lower—and more easily manage—their out-of-pocket prescription drug costs. That’s due to a new Medicare Part D Payment Plan that takes effect in January 2025.
Medications that prevent, rather than just treat, migraine attacks are now recognized as a first-line treatment for patients. The American Headache Society recognized CGRP – or calcitonin gene-related peptide – inhibitors as a new go-to treatment in updated 2024 guidance.
Step therapy was front and center at the eighth annual Capitol Hill Policy Forum, hosted in March 2024 by The Headache & Migraine Policy Forum (HMPF) and the Alliance for Headache Disorders Advocacy (AHDA).
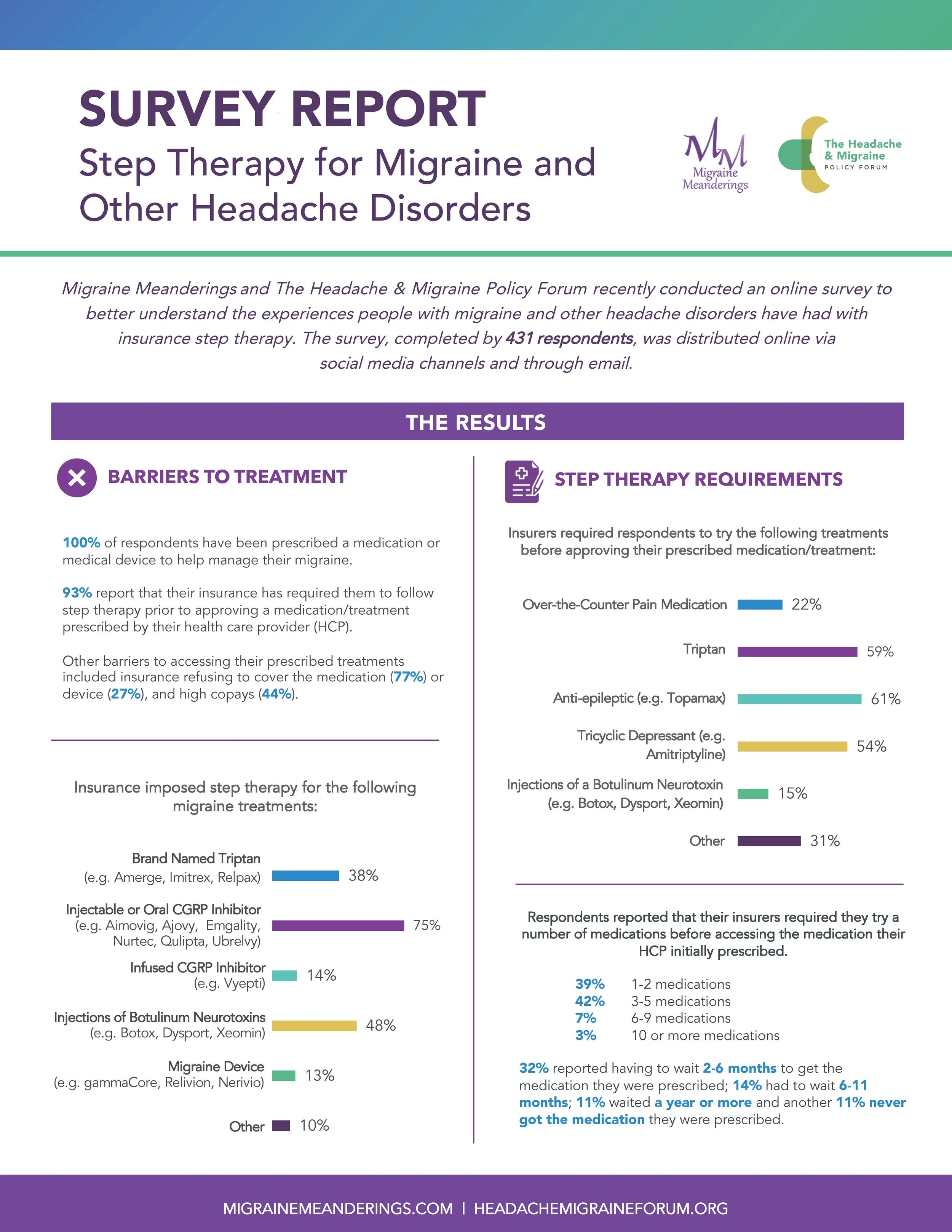
Health insurance plans may frequently delay, deny or change physician-prescribed treatments. New data from the Headache & Migraine Policy Forum and Migraine Meanderings exposes the impact of these insurance policies on patients' lives. Four patient surveys investigated the impact of prior authorization, step therapy, non-medical and the need for combination therapy.
Migraine Meanderings and The Headache & Migraine Policy Forum partnered together to ask the migraine community how their insurance coverage impacted their ability to access doctor-prescribed treatments for migraine.
Q: What is your typical virtual visit like?
After years of trying different treatment options, I now have my migraine well managed.
If your insurer denies coverage for your prescribed migraine treatment, you can appeal their decision. Follow these steps.
On June 21, 2023, the Partnership to Advance Cardiovascular Health, The Headache & Migraine Policy Forum and the Derma Care Access Network co-hosted a briefing on pharmacy benefit managers at the United States Capitol.
Migraine Meanderings and The Headache & Migraine Policy Forum recently conducted an online survey to better understand the experiences people with migraine and other headache disorders have had with insurance step therapy. The survey, completed by 431 respondents, was distributed online via social media channels and through email.
Long COVID-19 poses a growing and complex challenge for the headache and migraine community. For about one in five long-COVID patients, headache is among the symptoms that linger after acute COVID-19 infection subsides.
Migraine Meanderings and The Headache & Migraine Policy Forum recently conducted an online survey to better understand if and how people with migraine and other headache disorders are using medical devices. The survey, completed by 326 respondents, was distributed online via social media channels and through email.
Migraine is a disabling disease. So it’s important to select a health plan that covers the full range of treatment options that you need.
Migraine Meanderings and The Headache & Migraine Policy Forum recently conducted an online survey to better understand the experience people with migraine have with combination therapy for migraine. The survey received 516 responses gathered via social media and email.
Severe throbbing pain, nausea, extreme sensitivity to light and sound — these life-disrupting symptoms are all too familiar to people living with migraine disease. Thanks to medical research and innovation, migraine patients have never had more treatment options. Intravenous infused medications recently expanded those options by offering fast, effective relief that other treatments cannot always provide.
Migraine Meanderings and The Headache & Migraine Policy Forum recently conducted an online survey to better understand the experience people with migraine have in the emergency room and urgent care. Five hundred responses were gathered via social media and email.
Migraine is a disabling neurological disease affecting nearly 40 million Americans. While attacks can sometimes seem to come out of nowhere, patients may come to recognize triggers, which can vary from person to person.
Debilitating headache disorders and migraine disease affect 40 million Americans. When health plans empower those people to manage their disease, everyone benefits – patients, families, communities, workplaces and the health care system at large.
For some U.S. veterans and 9/11 first responders, the long-term impact of service takes the form of debilitating and chronic headache disorders. But the health care these men and women rightly deserve is often out of reach.
National Survey Results on How Federal Requirements Impact Access to Botulinum Toxins
A national survey of nearly 300 patients and health care providers throughout the United States explores how the Centers for Medicare and Medicaid Services’ requirement for prior authorization before each botulinum toxin treatment is limiting access, creating treatment delays and causing patients to struggle unnecessarily.
More than 1 in 10 women, men and children in the United States live with migraine disease. How does the ongoing COVID-19 pandemic impact their health and ability to receive optimal care?
To explore this question, The Headache and Migraine Policy Forum, in partnership with Migraine Again, conducted a national survey of more than 1,000 migraine patients throughout the United States.
A discussion with Carrie Dougherty, MD
Q. How is the stress of the COVID-19 pandemic impacting migraine patients?
In July 2019, HealthyWomen convened a two-day, multi-stakeholder meeting to identify knowledge gaps and challenges in treating and managing chronic pain in women: Science, Innovation and Technology Summit: Chronic Pain in Women—Focus on Treatment, Management and Barriers. The goal was to advance and elevate the current dialogue on effectively treating and managing chronic pain in women by addressing the numerous disparities, sex differences and stigma associated with chronic pain in women. Clinical professionals, researchers and policymakers, as well as representatives from federal agencies, industry, nonprofit organizations and advocacy groups attended, including several women who have been living with chronic pain for decades.
Can the more than 47 million Americans with migraine and headache disorders access the specialized care they need?
A 2020 Capitol Hill panel convened by The Headache & Migraine Policy Forum gathered patients, providers, advocates and policymakers to discuss how the shortage of headache specialist impacts patient care. The event coincided with the 13th annual Headache on the Hill congressional advocacy event, organized by the Alliance for Headache Disorders Advocacy.
Migraine disease has a far-reaching societal impact and significant economic consequences. In fact, it is one of many factors contributing to the gender wage gap in America. But it doesn’t have to be this way. Learning the facts about migraine disease and how employers can improve conditions for persons living with migraine can have a profound impact on women and workplaces across America.
A 2019 Capitol Hill policy panel convened by The Headache & Migraine Policy Forum brought together patients, health care providers, advocates and policymakers to consider this and related questions on migraine disease, disability and employment in the United States. The event coincided with the 12th annual Headache on the Hill congressional advocacy event, organized by the Alliance for Headache Disorders Advocacy.
More than “just a headache,” migraine is a hereditary neurological disease that affects people both physically and mentally. In addition to the pain of migraine attacks, the disease negatively affects patients’ ability to work, social relationships with family and friends, and the ability to provide basic self-care and to undertake normal life activities.
The story has become a familiar one. A patient with a chronic condition works with his or her doctor to find the right treatment.
The condition is stabilized, manageable. But then that stable patient is driven by the insurance company to a drug that’s less expensive. The switch prioritizes insurers’ profit over patients’ health. And it often comes with consequences: new side effects, re-emerging symptoms that had been under control, or interactions with medication the patient takes for other conditions.
An August 2018 attitudinal survey of more than 340 female migraine stakeholders from throughout the United States revealed clear opinions about the debilitating impact of migraine and headache disorders – and a lack of faith in health insurers and employers to properly meet the needs of people with the disease.
Imagine living with the debilitating pain of chronic migraine, the annoyance of excessive perspiration, or the embarrassment of involuntary neck twisting and jerking. Patients who experience these conditions may benefit from treatment with a biologic.
A 2018 Capitol Hill policy panel sponsored by The Headache and Migraine Policy Forum brought together experts from across the health care and veterans support spectrum to consider this and related questions. The forum coincided with the 11th annual Headache on the Hill advocacy day, sponsored by the Alliance for Headache Disorders Advocacy.
Chronic migraine commonly characterized by headaches that occur on 15 or more days a month for at least three months is a disabling disease. Studies have shown that chronic migraine patients have impaired socioeconomic status, reduced quality of life and reduced workplace productivity.
Balanced pain management is a comprehensive approach to diagnosing, treating and controlling pain that ensures practitioners and their patients, not insurance companies or other outside parties, drive treatment decisions. It better alleviates pain by giving people access to the full range of effective treatment strategies.